Integrative Approach to Osteoarthritis
Dr. Tatyana's Health and Wellness Blog
Treating the whole person to restore optimal health. Check back often for up-to-date news and information about acupunture and Chinese medicine.
Most Recent Posts ...
Posted on: 12/8/2025
Posted on: 11/24/2025
Posted on: 11/10/2025
Posted on: 10/27/2025
Search All Blog Posts
Blog Post Archive Categories
- Top 5 Ways to Stay Healthy This Winter and Avoid the Flu
- Happy Thanksgiving: A Season of Gratitude, Healing & Reflection
- Salt Room Therapy: Your Sanctuary for Breathing, Healing & Deep Relaxation
- Quieting the Storm: How Acupuncture and Neurofeedback Can Help Functioning Alcoholics Break Free
- How Acupuncture Can Help Restore Menstrual Health in Amenorrhea
- How Acupuncture Can Help Reduce Fear and Anxiety Caused by Stress
- Chronic Fatigue and Chronic Inflammation: A Holistic Look Through Western and Eastern
- The Hidden Dangers of Overusing Supplements: Are You Taking More Than You Should?
- The Importance of Exercise and How to Stay Motivated for a Healthier You
- Jameson, J. L., Fauci, A. S., Kasper, D. L., Hauser, S. L., Longo, D. L., Jameson, J. L., … Harrison, T. R. (2018). Harrison's principles of internal medicine.
- Johnson VL, Hunter DJ. The epidemiology of osteoarthritis. Best Pract Res Clin Rheumatol. 2014;28(1):5–15. doi: 10.1016/j.berh.2014.01.004.
- Maciocia, G. (1997). The practice of Chinese medicine: The treatment of diseases with acupuncture and Chinese herbs. Edinburgh: Churchill Livingstone.
- Au, K. Y., Chen, H., Lam, W. C., Chong, C. O., Lau, A., Vardhanabhuti, V., … Lao, L. (2018). Sinew acupuncture for knee osteoarthritis: study protocol for a randomized sham-controlled trial. BMC Complementary and Alternative Medicine, 18, 133. http://doi.org/10.1186/s12906-018-2195-8
- Witt C, Brinkhaus B, Jena S, Linde K, Streng A, Wagenpfeil S, Hummelsberger J, Walther HU, Melchart D, Willich SN. Acupuncture in patients with osteoarthritis of the knee: a randomised trial. Lancet. 2005;366(9480):136–143. doi: 10.1016/S0140-6736(05)66871-7.
- Corbett MS, Rice SJC, Madurasinghe V, Slack R, Fayter DA, Harden M, Sutton AJ, MacPherson H, Woolacott NF. Acupuncture and other physical treatments for the relief of pain due to osteoarthritis of the knee: network meta-analysis. Osteoarthr Cartilage. 2013;21(9):1290–1298. doi: 10.1016/j.joca.2013.05.007
- Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part II: OARSI evidence-based, expert consensus guidelines. Osteoarthr Cartil. 2008;16(2):137–162. doi: 10.1016/j.joca.2007.12.013
- Berman BM, Lao LX, Langenberg P, Lee WL, Gilpin AMK, Hochberg MC. Effectiveness of acupuncture as adjunctive therapy in osteoarthritis of the knee - a randomized, controlled trial. Ann Intern Med. 2004;141(12):901–910. doi: 10.7326/0003-4819-141-12-200412210-00006.
- White A, Foster NE, Cummings M, Barlas P. Acupuncture Treatment for Chronic Knee Pain: A Systematic Review. Rheumatology (Oxford) 2007;46:384–390.
- Manheimer E, Cheng K, Linde K, Lao L, Yoo J, et al. Acupuncture for Peripheral Joint Osteoarthritis. Cochrane Database Syst Rev. 2010:CD001977
Integrative Approach to Osteoarthritis
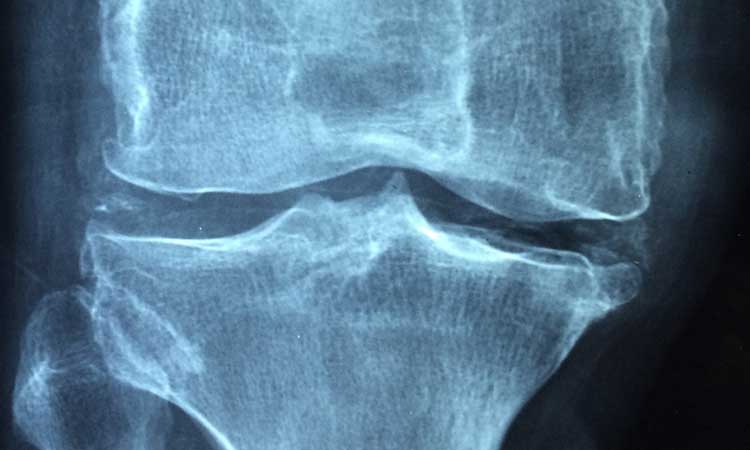
Osteoarthritis (OA), or degenerative arthritis (degenerative joint disease), is the most common form of joint problems and progresses with aging. As a result, it is also called “wear-and-tear” disease. In the United States, osteoarthritis prevalence is expected to increase by 66%–100% by 2020. People with obesity have a higher risk of developing OA (1). OA most commonly affects joints in the hip, knee, and spine (cervical and lumbosacral area) as well as the first metatarsals pharyngeal joints. OA starts with structural changes in the joints, including cartilage loss and the formation of osteophytes. In knees, meniscal degeneration is part of the disease. X-rays are the most common diagnostic tool used to confirm OA. Sometimes abnormal changes (joint deformation) can be found without clinical presentation. The diagnosis of symptomatic OA of the knee occurs in approximately 12% of those older than 60 in the United States and approximately 6% of adults at least 30 years old (1,2).
Ligaments, cartilage, muscles, and joint capsules play a critical role in protecting the joints, and all are involved in the development of the disease. The primarily targeted tissue for this disease is cartilage. It is lubricated by the synovial fluid to provide the best movement. In OA, osteophytes form, and the cartilage gradually loses aggrecan (the collagen matrix) and type-two collagen, leading to stiffness. Inflammation in the joint can occur, but as a secondary pathological response. The progression of the disease starts when cartilage loses its elasticity and can be damaged very easily; the resulting loss of cartilage leads to damage to the underlying bone. Bony growth or osteophytes then develop in the affected bone. The synovium becomes inflamed due to the cartilage breakdown, causing cytokines and enzymes that lead to more damage of the cartilage (3). Systemic factors affecting joints are age, female gender (connected to menopause), nutritional factors, previous damage, muscle weakness, incising bone density, and proprioceptive deficiency. Usually the combination of loading and systemic factors is necessary to cause OA and its progression.
According to traditional Chinese medicine (TCM), OA (called “Cold Bi Syndrome”) is often accompanied by an underlying kidney yang deficiency (usually declining with age) and/or spleen qi deficiency and damp accumulation. As the disease progresses, it leads to Cold Bi Syndrome. The formation of Bone Bi Syndrome is the most painful stage, with the most limited range of motion. According to TCM, the cold and damp weather can aggravate all symptoms of osteoarthritis (3).
The most common clinical symptoms in OA are joint pain, which worsens with movement; stiffness, especially in the morning; a limited range of motion; joint deformation; tender spots; osteophytes; and swelling, which is typical in long-term conditions. Pain relief is normally achieved by using warm pads.
The main target principles for the treatment of OA are to stop and prevent tissue damage, improve cartilage regeneration, minimize the occurrence of disability, reduce pain, and increase the range of motion, thereby minimizing disability.
According to OARSI’s evidence-based, expert consensus guidelines, the optimal management of patients with OA in the hip or knee requires a combination of non-pharmacological and pharmacological modalities of therapy. Non-pharmacological modalities include education and self-management; regular telephone contact; referral to a physical therapist; aerobic, muscle strengthening, and water-based exercises; weight reduction; walking aids; knee braces; footwear and insoles; thermal modalities; transcutaneous electrical nerve stimulation; and acupuncture.
Pharmacological modalities of treatment include acetaminophen, cyclooxygenase-2 (COX-2) non-selective and selective oral non-steroidal anti-inflammatory drugs (NSAIDs), topical NSAIDs and capsaicin, intra-articular injections of corticosteroids and hyaluronates, glucosamine, and/or chondroitin sulphate for symptom relief; glucosamine sulphate, chondroitin sulphate, and diacerein for possible structure-modifying effects; and the use of opioid analgesics for the treatment of refractory pain. Recommendations cover five surgical modalities: total joint replacement, uni-compartmental knee replacement, osteotomy and joint-preserving surgical procedures, joint lavage and arthroscopic debridement in knee OA, and joint fusion as a salvageprocedure when joint replacement has failed (7). The limitations of these medications are that they may damage the kidneys, cardiovascular system, and gastrointestinal tract. Long-term use is not recommended due to these harmful side effects. It is very beneficial to start preventative care with a non-pharmacological approach first. In some acute cases, medications can be used for a short period of time.
Acupuncture is a safe and effective approach to treating OA. Research shows that performing acupuncture once a week for 6 weeks can safely relieve pain and symptoms of knee osteoarthritis (KOA) and improve patients’ functional movement and quality of life (4). One study with 294 participants (5) found that, after 8 weeks of treatment, pain and joint function improved more with acupuncture than with minimal acupuncture or no acupuncture in patients with osteoarthritis of the knee.
Efforts have also been made to determine whether acupuncture provides greater pain relief and improved function compared to sham acupuncture or education in patients with osteoarthritis of the knee. “The true acupuncture group experienced significantly greater improvement than the sham group in the WOMAC function score (mean difference, -2.5 [CI, -4.7 to -0.4]; P = 0.01), WOMAC pain score (mean difference, -0.87 [CI, -1.58 to -0.16]; P = 0.003), and patient global assessment (mean difference, 0.26 [CI, 0.07 to 0.45]; P = 0.02)” (8).
Three recent reviews, including a systematic review, a Cochrane review, and a meta-analysis, evaluated the effects of acupuncture in osteoarthritis compared to no acupuncture and sham acupuncture with mixed results. The systematic review concluded that acupuncture is significantly superior to sham acupuncture in improving pain and functions in patients with OA (9). The latest Cochrane review, including 16 randomized trials, indicated that, when compared with waiting-list controls, acupuncture recipients showed statistically and clinically significant short-term improvements in pain and functions among those with OA. Compared to sham
controls, acupuncture provided small, statistically significant improvements (10). In comparison, regarding the effectiveness of acupuncture with other relevant physical treatments for alleviating pain due to knee osteoarthritis, currently available network meta-analysis results indicated that acupuncture can be considered one of the more effective physical treatments for alleviating osteoarthritis knee pain in the short-term (6). In order to have a positive long-term result, acupuncture treatments should be performed continuously and weekly, which is not possible some patients with limited financial abilities.
In summary, the pathophysiological basis of OA is complex and multifaceted, and symptomatic OA is heterogeneous. Integrative approaches combine the best of conventional medicine and acupuncture therapies to ultimately improve patient care. These modalities may lead to the development of better disease-modifying strategies that could improve symptoms and decrease OA progression. More clinical trials with acupuncture treatment must be conducted to prove the long-term effects.
References:




